Título
Autor
Fecha
Lugar de Realización
Texto
Endoscopic Treatment of Posterior Fossa Arachnoid Cysts
Yusuf Ersahin
Division of Pediatric Neurosurgery Ege University Faculty of Medicine Izmir, Turkey
Correspondencia: Division of Pediatric Neurosurgery, Ege University Faculty of Medicine Bornova, Izmir 35100 Turkey
E-mail: ersahin@med.ege.edu.tr
RESUMEN
Objetivo. Presentar los resultados del tratamiento endoscópico de los quistes aracnoideos de la fosa posterior.
Material y método. Se revisan las historias de pacientes tratados entre los años 2000 y 2004 evaluando edad, sexo, hallazgos radiológicos y tratamiento previo. En todos los procedimientos se utilizó un endoscopio rígido.
Resultados. Encontramos 6 niños y 3 niñas (edad promedio 29,9 meses) La fenestración endoscópica de los quistes fue útil en 7 de los 9 pacientes. De los 4 pacientes a los que se había implantado válvulas previamente, 3 no requirieron derivación.
Conclusión. El tratamiento endoscópico de los quistes aracnoideos de la fosa posterior debe ser el de primera opción en las instituciones que hagan esta práctica de rutina.
Palabras clave: fosa posterior, neuroendoscopia, quiste aracnoideo
ABSTRACT
Objectives. The aim of this paper is to present the results of endoscopic intervention in retrocerebellar arachnoid cysts.
Material and methods. The patients with posterior fossa arachnoid cysts in which a neuroendoscopic intervention had been done between 2000 and 2004 were retrospectively reviewed. Age, gender, presenting symptoms and signs, radiologicalfindings and previous modes of treatment were evaluated. A rigid neuroendoscope was used in all procedures.
Results. There were 6 boys and 3 girls who ranged in age from 1 month to 16 years (mean 29.9 months). Endoscopic cyst fenestration was successful in 7 of 9 patients. Of the 4 patients who had been previously shunted, 3 became shunt free.
Conclusion. Endoscopic cysto-cisternostomy should be the first step in the management of posterior fossa arachnoid cyst in the institutions where neuroendoscopy is routinely practiced.
Key words: neuroendoscopy, arachnoid cyst, posterior cranial fossa
INTRODUCTION
Arachnoid cysts are usually developmental lesions, which may occur wherever cerebrospinal fluid (CSF) and arachnoid membranes are present. There are different opinions on the management of intracranial arachnoid cysts in terms of both the surgical indications and the mode of surgical intervention. The aim of this paper is to present the results of endoscopic intervention in retrocerebellar arachnoid cysts.
MATERIAL AND METHODS
The patients with posterior fossa arachnoid cysts in which a neuroendoscopic intervention had been done between 2000 and 2004 were retrospectively reviewed. The patients with quadrigeminal plate, cerebello-pontine angle and clival arachnoid cysts were excluded. Age, gender, presenting symptoms and signs, radiological findings and previous modes of treatment were evaluated. A rigid neuroendoscope was used in all procedures.
When the patient's symptoms and signs have improved and the patient has not needed further surgeries such as shunting or open surgery, the endoscopic intervention was considered as successful.
The diagnosis of arachnoid cyst was made by magnetic resonance imaging (MRI) in all patients. Patients had a computed tomography (CT) within several hours after endoscopic surgery to rule out complications. Postoperative T2-weighted MRI was done to show signal voids through opening between the cisterna magna and cyst (Fig. 1).
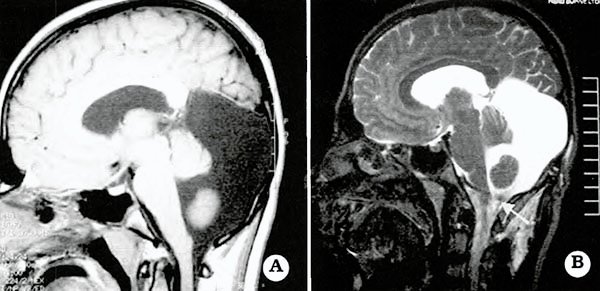
Fig. 1. A. Preoperative T1- weighetd sagittal MRI showing retrocerebellar arachnoid cyst. B. Note theflow void (arrow) through cystocisternostomy on postoperative T2-weighted sagittal MRI.

Fig. 2. A. Endoscopic photograph showing the cerebellar hemispheres and inferior border of the cyst. B. Bipolar coagulation of the inferior wall of the cyst. C. Balloon dilatation of the fenestration. D. Fenestration of the inferior cyst wall (cysto-cisternostomy). E. Visualization of the lower cranial nerves and the spinal cord by the rigid neuroendoscope.
Technique
All patients were operated on under general anesthesia in prone position. A vertical paramedian skin incision, 3-4 cm in length is done in the suboccipital region. The side in which the arachnoid cyst is larger was used. A very small craniotomy (1.5 cm x 2 cm) below the transverse sinus is performed, since a small burr hole does hinder the rigid neuroendoscope from moving obliquely and accessing the cisterna magna. The dura is linearly incised and zero degree straightforward rigid neuroendoscope (Karl Storz, Tutlingen, Germany and Channel Neuroendoscope, Medtronic, Minneapolis, MN) is inserted into the cyst after the cyst is punctured. A cysto-cisternostomy is performed between the cyst and cisterna magna. The lower cranial nerves and the spinal cord are visualized (Fig. 2). At the end of the procedure the dural incision is either primarily sutured or grafted with a collagen matrix (DuraGen, Integra LifeSciences Corporation, New Jersey, U.S.A.)
RESULTS
Nine patients with posterior fossa arachnoid cyst underwent an endoscopic procedure. Six boys and 3 girls ranged in age from 1 month to 16 years (mean 29.9 months) (Table 1). In 3 patients, posterior fossa cyst was diagnosed by ultrasound before birth. Five patients were delivered by cesarean section and 4 had a normal vaginal delivery.
Macrocrania was the most common presenting symptom and sign. All patients had a noncommunicating hydrocephalus. Four patients who had been previously shunted at another hospital, presented with headache, vomiting or symptoms of intracranial hypertension at the time of shunt malfunction.
Table 1: Summary of the patients with retrocerebellar arachnoid cysts.

Ventriculo-peritoneal (VP) shunt and cysto-peritoneal (CP) shunt had been inserted in 2 and 2 patients, respectively. In one of the patients, we had to reinsert a CP shunt, following both endoscopic fenestration and cyst excision by open surgery. When this patient had been on external drainage befo-re open surgery, more than 750 ml CSF per day were excreted to the drainage bag.
A repeat endoscopic fenestration was performed in one of the patients almost 2 years after the initial endoscopic intervention. Of the 4 patients with shunts, 3 became shunt free. Endoscopic cyst fenestration was successful in 7 of 9 patients. Postoperative subcutaneous CSF collection and fistula occurred in two and one patient, respectively. Two of the 3 patients with complication did not benefit from endoscopic cyst fenestration. A reduction in cyst size in varying degrees and a signal void through fenestration between the cisterna magna and cyst were shown on the postoperative MRI scans of the 7 patients (Fig. 3). In 2 patients, there was no change in cyst volume and ventricular dilatation increased and a CP shunt was inserted. The follow-up ranged from 3 to 51 months (mean 26.4 months).

Fig. 3. A. Preoperative T1-weighted MRI scans showing a retrocerebellar arachnoid cyst. B. Postoperative showing a reduction in the cyst volume and some expansion of the cerebellar hemispheres.
DISCUSSION
Arachnoid cysts are occasionally encountered in the posterior fossa. Infratentorial arachnoid cysts may be retrocerebellar, supravermian (supracollicular) or in the cerebellopontine angle1,2. However, we included only retrocerebellar arachnoid cyst in this series. Megacisterna magna, Dandy-Walker syndrome, cerebellar hypoplasia, hydrocephalus in the presence of a non-spaceoccupying retrocerebellar CSF collection, dermoid or epidermoid cysts, cystic cerebellar astrocytoma and cerebellar hemangioblastoma should be taken into consideration in differential diagnosis1,3-5. Galassi et al6 reported that posterior fossa arachnoid cysts affect males more than females and may become symptomatic at any age and a history of a difficult or traumatic delivery was present in half of the cases. Six of the nine children were male in our series and all presented with hydrocephalus in their infancy. There were eight female and four male patients in the series of Samii et al7. No sex difference has been reported by others3. Posterior fossa cyst was diagnosed prenatally in 3 of the 9 patients and five patients were delivered by cesarean section and 4 had a normal vaginal delivery.
Endoscopic treatment of arachnoid cysts has been infrequently reported8-14. Endoscopic treatment of midline supratentorial arachnoid cysts such as suprasellar arachnoid cyst has been accepted as a choice of treatment by most of the neurosurgeons8,10,14,17. However, the experience on the endoscopic treatment of arachnoid cysts in the posterior fossa is limited. Schroeder et al14 performed endoscopic cysto-cisternostomy in 2 patients with posterior fossa arachnoid cysts and the clinical improvement and cyst reduction were achieved in both patients. Hopf and Perneczky10 endoscopic neurosurgery in 2 and endoscopeassisted microneurosurgery in 1 patient with retrocerebellar arachnoid cysts. Of 3 patients, 2 improved clinically although cyst reduction was determined in only one patient. However, they reported that the best success rates were achieved in patients with intraventricular cysts (89%) and posterior fossa arachnoid cysts (78%) including quadrigeminal, cerebellopontine angle, supra and retrocerebellar cysts. Choi et al8 carried out cystocisternostomy in 5 arachnoid cysts in the posterior fossa and cyst reduction was achieved in 3. They did not find any case of reclosure of the fenestration site in any of the patients who underwent successful endoscopic procedure without hemorrhage or infection in a series of 36 patients with congenital arachnoid cysts. They also think that reclosure of the fenestration site may be related to hemorrhage or infections.
In the series of 7 patients with arachnoid cysts reported by Kim11, the cerebellar arachnoid cyst disappeared following endoscopic fenestration. Gangemi et al9 reported a successful result in 2 patients with posterior fossa arachnoid cyst in which endoscopic cyst fenestration and endoscope-assisted microneurosurgery had been done. A 32-year-old with an arachnoid cyst of the posterior fossa manifesting as cervical syringomyelic myelopathy improved following endoscopic cyst fenestration. The inferior wall of the cyst was disturbing CSF pulsatile movement between the in traspinal and intracranial subarachnoid spaces12. The symptoms and signs of intracranial hypertension were relieved by endoscopic cyst fenestration in 7 of the nine patients with a retrocerebellar arachnoid cyst in our series. One of the patients had a repeat endoscopic cystocisternostomy. This patient had had shunt infection before the first endoscopic procedure was done. The other patient in whom the endoscopic cyst fenestration failed had been previously shunted. He had CSF fistula through the skin incision after the endoscopic cyst fenestration and an external drain was inserted in the cyst because of infection. The daily amount of CSF, drained in the drainage bag was greater than 750 ml. Although a cyst excision was performed by craniotomy, he needed a CP shunt. CSF production by enclosed ectopic choroid plexus is one of the mechanisms of cyst growth18.19. Such a mechanism may account for a high rate of CSF production in our patient.
No major complication following endoscopic surgery in posterior fossa arachnoid cysts has been reported8-12,14. The complications of open surgery are more frequent and severe20-22. However, open surgery and radical removal of the arachnoid cyst in the posterior fossa can be safe and effective in experienced hands3,7. Shunt surgery has no mortality and very low complication rate. A marked reduction in cyst size is almost always seen on CT or MRI after shunting21,23. Shunt dependency and complications are inevitable in the long term24.
The number of the cases who underwent endoscopic cyst fenestration is small. We need to have a larger number of patients to prove the effectiveness of endoscopic intervention in posterior fossa arachnoid cysts. However, the results of endoscopic surgeries reported in the literature so far are promising. Endoscopic cysto-cisternostomy should be the first step in the management of posterior fossa arachnoid cyst in the institutions where neuroendoscopy is routinely practiced.
References
1. Boltshauser E, Martin F, Altermatt S: Outcome in children with space-occupying posterior fossa arachnoid cysts. Neuropaediatrics 2002; 33: 118-21.
2. Naidich TP, McLone DG, Radkowski MA. Intracranial arachnoid cysts. Pediatr Neurosci 1985-86; 12: 112-22.
3. Erdincler P, Kaynar MY, Bozkus H, Ciplak N. Posterior fossa arachnoid cysts. Br J Neurosurg 1999; 13: 10-17.
4. Gosalakkal JA: Intracranial arachnoid cysts in children: A review of pathogenesis, clinical features, and management. Pediatr Neurol 2002; 26: 93-8.
5. Rock JP, Zimmerman R, Bell WO, Fraser RAR: Arachnoid cysts of the posterior fossa. Neurosurgery 1986; 18: 176-9.
6. Galassi E, Tognetti F, Frank F, Fagioli L, Nasi MT, Gaist G. Infratentorial arachnoid cysts. J Neurosurg 1985; 63: 210-7.
7. Samii M, Carvalho GA, Schuhmann MU, Matthies C: Arachnoid cysts of the posterior fossa. Surg Neurol 1999; 51: 376-82.
8. Choi JU, Kim DS, Huh R: Endoscopic approach to arachnoid cyst. Childs Nerv Syst 1999; 15: 28591.
9. Gangemi M, Maiuri F, Colella G, Sardo L: Endoscopic surgery for large posterior fossa arachnoid cysts. Minim Invasive Neurosurg 2001; 44: 21-4.
10. Hopf NJ, Perneczky A: Endoscopic neurosurgery and endoscope-assisted microneurosurgery for the treatment ofintracranial cysts. Neurosurgery 1998;
43: 1330-6.
11. Kim M-H: The role of endoscopic fenestration procedures for cerebral arachnoid cysts. J Korean Med Sci 1999; 443-7.
12. Nomura S, Akimura T, Imoto H, Nishizaki T, Suzuki M: Endoscopic fenestration of posterior fossa arachnoid cyst for the treatment of presyrinx myelopathy-case report. Neurol Med Chir (Tokyo) 2002; 42: 452-4.
13. Schônherr B, Wolf O, Meier U: Endoscopy of intracranial cyst in the adult patient. Minim Invasive Neurosurg 2002; 45: 181-4.
14. Schroeder HW, Gaab MR, Niendorf WR: Neuroendoscopic approach to arachnoid cysts. J Neurosurg 1996; 85: 293-8.
15. Caemert J, Abdullah J, Calliauw L, Carton D, Dhooge C, van Coster R: Endoscopic treatment of suprasellar arachnoid cysts. Acta Neurochir (Wien) 1992; 119: 68-73.
16. Decq P, Brugiéres P, Le Guerinel C, Djindjian M, Kéravel Y, Nguyen J-P: Percutaneous endoscopic treatment of suprasellar arachnoid cysts: ventriculocystostomy or ventriculocystocisternostomy? Technical note. J Neurosurg 1996; 84 :696-701.
17. Kirollos RW, Javadpour M, May P, Mallucci C: Endoscopic treatment of suprasellar and third ventricle-related arachnoid cysts. Child's Nerv Syst 2001; 17: 713-8.
18. Iglesias JR, Sanjuanbenito L, Martinez-Cubells J, Lousa M, Redondo C: Intracerebral arachnoidal cyst containing choroid plexus. Case report. Acta Neurochir (Wien) 1981; 58: 229-34.
19. Schuhmann MU, Tatagiba M, Hader C, Brandis A, Samii M: Ectopic choroid plexus within a juvenile arachnoid cyst of the cerebellopontine angle: cause of cyst formation or reason of cyst growth. Pediatr Neurosurg 2000; 32: 73-6.
20. Aoki N, Sakai T: Intraoperative subdural hematoma in a patient with arachnoid cysts in the middle cranial fossa. Child's Nerv Syst 1990; 6: 44-6.
21. Ciricillo SF, Cogen PH, Harsh GR, Edwards MSB: Intracranial arachnoid cysts in children. A comparison of the effect of fenestration and shunting. J Neurosurg 1991; 74: 230-5.
22. Stein SC: Intracranial developmental cysts in children: treatment by cystoperitoneal shunting. Neurosurgery 1980; 8: 647-50.
23. McBride LA, Winston KR, Freeman JE: Cystoventricular Shunting of Intracranial Arachnoid Cysts. Pediatr Neurosurg 2003; 39: 323-9.
24. Kim S-K, Cho B-K, Chung Y-N, Kim H-S, Wang K-C: Shunt dependency in shunted Arachnoid cyst: a reason to avoid shunting. Pediatr Neurosurg 2002; 37: 178-85.
